BLOG
I denti: l’unica parte del corpo che non guarisce da sola
Il corpo umano è una macchina biologica incredibilmente complessa, con una straordinaria capacità di autoguarigione....
Quando il dentista diventa un luogo accogliente: la sensazione di essere a casa
Perchè andare dal dentista dev’essere fonte di ansia e paura? Lo studio dentistico Pinzuti ha creato un luogo accogliente e confortevole per un’esperienza senza timori e piacevole
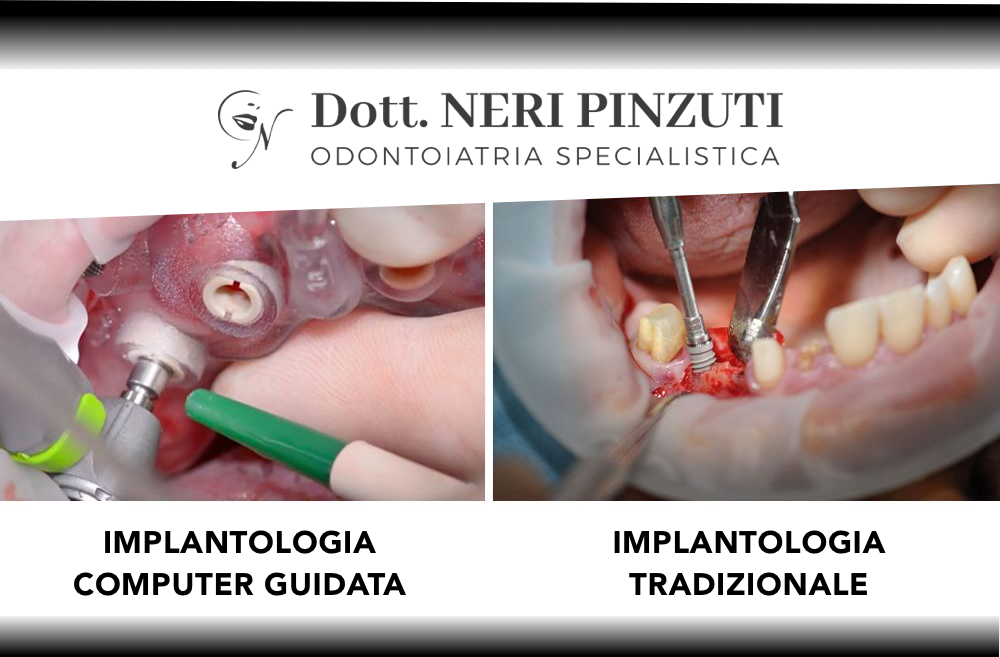
Basta bisturi con l’implantologia computer guidata minimamente invasiva
Implantologia computer guidata minimamente invasiva La perdita dei denti naturali è un fenomeno fortemente...
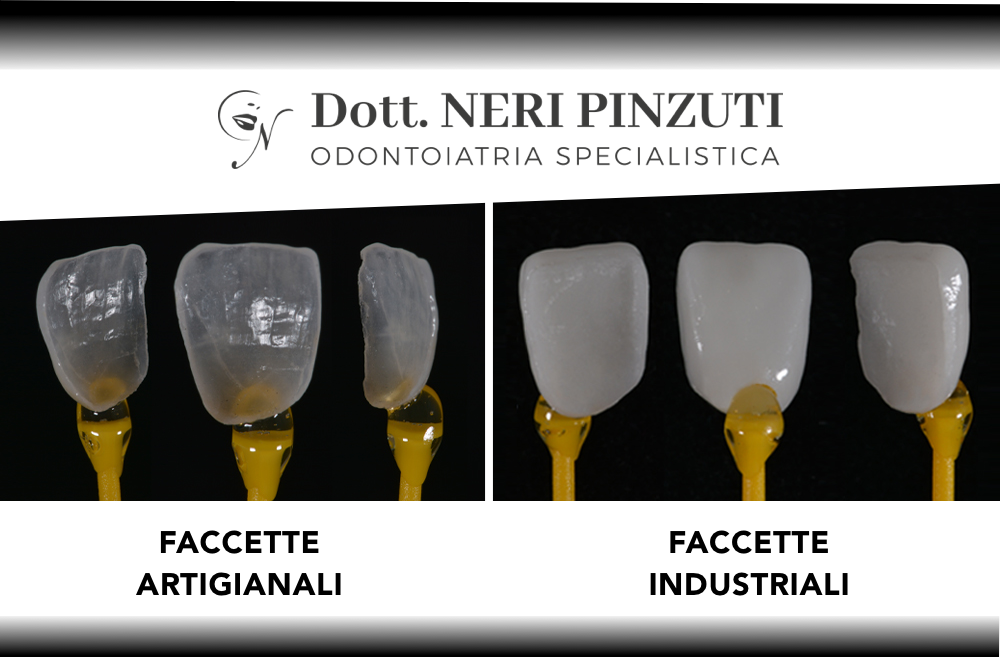
La nuova era delle faccette dentali
BASTA LIMATURA E MATERIALI A EFFETTO DENTIERA. OGGI LE FACCETTE SI REALIZZANO CON IL PLATINO PER UN EFFETTO NATURALE...
Sbiancamento dentale laser
Avere un bel sorriso con denti bianchi rappresenta il principale biglietto da visita nel determinare la prima...
L’odontoiatria estetica: migliorare il nostro sorriso senza provare dolore
Odontoiatria estetica Se è luogo comune avere paura del dentista, quando si pensa all’odontoiatria estetica si presume...
Dentista e dolore: come sfatare un mito
Intervista al Dott. Neri Pinzuti, specialista di Odontoiatria Estetica. Molte persone hanno paura di andare dal...
Centri low cost e turismo dentale: intervista a Neri Pinzuti
Il professionista Neri Pinzuti risponde alle più comuni domande sui centri dentistici low cost e sul cosiddetto...
Che cos’è la parodontite?
La parodontite è una patologia infettiva cronica (comunemente nota come piorrea) che causa la distruzione...
Denti e Photoshop? No, grazie
Nel contesto odierno, fatto di grandi aspettative del paziente e di contenziosi in aumento (con particolare riguardo...
L’importanza degli impianti dentali certificati: Fiat o Ferrari?
Un argomento spesso poco dibattuto verte intorno alla qualità degli impianti dentali e le certificazioni che il...
Scegliere un sorriso low cost? Il caso di Ornella
Si parla ormai sempre più spesso di centri low cost e cure odontoiatriche a basso prezzo, in grado di garantire...
L’importanza dei controlli odontoiatrici: ogni quanto devono essere effettuati?
Controlli odontoiatrici: spesso pensiamo di avere una bocca in piena salute perché non si avverte alcun dolore o non...
Come scegliere un buon dentista?
La crisi economica e la nascita di studi odontoiatrici low cost hanno determinato un aumento notevole dei dentisti,...
10 motivi per stare alla larga dai centri dentistici low cost
Promettono sorrisi smaglianti low cost, pulizie dentali a 40€ e impianti tutto compreso per poche centinaia di euro....